
Advanced Physiological Optics Laboratory
Yoon Lab
There have been many studies to investigate what actually causes loss of accommodation with age, also called Presbyopia. To better understand the mechanism of accommodation and how it changes with age, the ability to image the entire anterior segment of the eye including cornea and crystalline lens is important. The same imaging technique can also assess the feasibility of accommodative intraocular lenses developed to restore accommodation. Four major technologies, Scheimpflug, VHF ultrasound, optical coherence tomography (OCT) and Magnetic Resonance Imaging (MRI) have been proposed. In our lab we are using OCT and MRI to image the anterior segment.
Our OCT system is a swept source OCT system using a Fourier Domain Mode Locked Laser to sweep wavelength, proposed by Huber et al. (Optics Express, 2005). Swept source OCT system provides faster image acquisition as well as better SNR when compared with a time domain OCT.
For a traditional OCT system with conventional scan geometry, it is very difficult to image the entire anterior segment (which includes two corneal surfaces and two lenticular surfaces) especially around peripheral areas at high contrast due to weak signal coming back. Our OCT system is equipped with a customized scanning system, which can shine light normal to the lenticular surfaces. Shining the light normal to the lenticular surfaces increases the amount of light scattered back. The scanning system could be divided into two halves: one optimized to achieve normal incidence angles on the two corneal surfaces and the front surface of the crystalline lens, and the other optimized to do the same for the back surface of the lens.
To evaluate the performance of our scanning design a model eye was constructed that consists of an artificial cornea and artificial lens made of PMMA. The dimensions in the model eye match exactly with the dimensions of the real eye. The lens in the model eye was submerged in water to imitate the aqueous of human eye.
Due to the non-telecentric nature of our scanning method, large amounts of distortion are expected in the images. The images obtained for the model eye using traditional scan (Fig 1a) and our scan design (Fig. 1 b and c) are shown in Fig 1. An average SNR improvement of 5dB and 12dB was obtained for the front and back surface, respectively. For the back surface of cornea SNR improvement of 4dB was observed while the SNR improvement for front surface of cornea was 0.4dB.
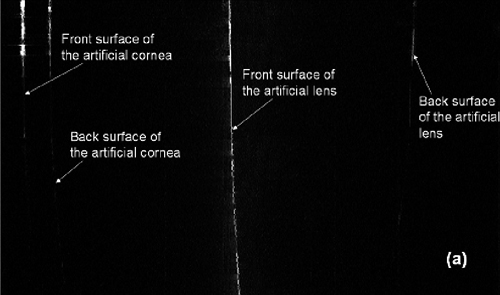
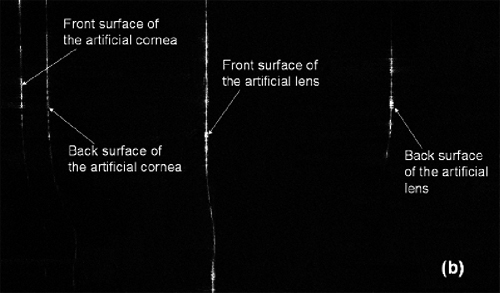
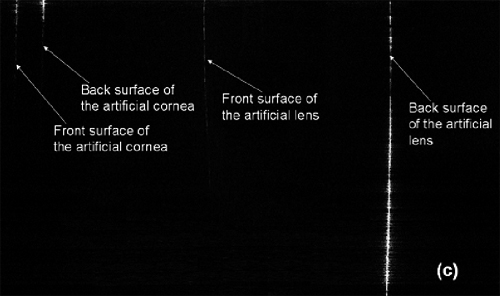
Figure 1: Images of the half of the eye obtained from (a) Custom Telecentric scan (b) Scan optimized for the front surface of the crystalline (c) Scan optimized for the back surface of the crystalline lens
The surface distortions were corrected by calculating the optical path differences in the ray tracing software as shown in Fig. 2. The dimensions obtained have some errors; these errors could be due to decentration and bending of the artificial cornea and lens.
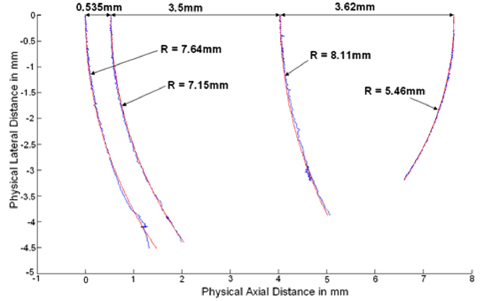
Figure 2: Distortion corrected image, blue curves represent the raw image and red curves are circular curves fitted to the raw data. The dimensions correspond to fitted curves.
We have shown an SNR improvement while imaging the model eye using our custom scanning optics, however we are yet to test the system in the real eye. Assuming we could get similar SNR improvement in the real eye, such a system can be a powerful tool for understanding the mechanism of accommodation and presbyopia and in evaluating the efficacy of accommodating intraocular lenses.
Current techniques being used to image the anterior chamber of the eye in vivo are Scheimpflug imaging, OCT, and high-frequency ultrasound. While these modalities have distinct advantages, they suffer from various drawbacks. In the case of ultrasound, an invasive impedance-matching gel is used on the eye and a relatively small penetration depth is imaged. Scheimpflug imaging and OCT are limited by the iris, which obscures the ciliary muscle body, zonluar fibers, and lens periphery. Imaging these peripheral structures of the anterior segment, which are responsible for applying and distributing the force necessary for accommodation, is of primary importance to understanding accommodation and presbyopia.
In collaboration with Rochester Center for Brain Imaging, our lab has developed an eye coil that allows for high-resolution MR images, in vivo.
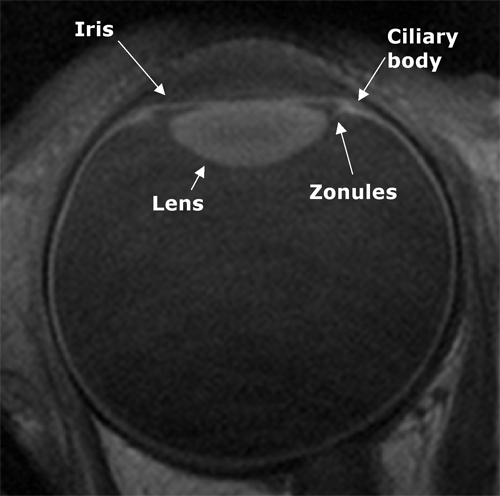
Figure 3: MR image of a pre-presbyopic eye at relaxed accommodation with 100μm axial and lateral resolution.
MRI is a useful tool because it images the entire ocular globe, enhancing our understanding of the mechanism of accommodation and presbyopia. Clinically, it is also a powerful tool for investigation of premium intraocular lens efficacy and restoration of accommodation.
It is our aim to use MRI to study the relationship between IOL axial displacement and ciliary ring diameter (contraction) as a function of naturally stimulated accommodation. This will clarify the impact of the ciliary muscle on the anterior and posterior shifts of IOL's as accommodation is stimulated and thus has direct impact on the development of new premium IOL designs.
Optical coherence tomography (OCT) is a leading biomedical imaging modality capable of generating images of living biological tissue in vivo at high resolution and has been widely used in the area of ophthalmology. Despite the benefits provided by OCT in studying eye diseases, origin and progression of many diseases are still difficult to investigate due, in part, to the lack of axial resolution that enables us to objectively quantify certain structures in the eye. Standard anterior segment OCT systems do not have sufficient axial resolution to precisely quantify the thickness of all the individual corneal layers. Hence, it has been increasingly important to further improve the axial resolution of the OCT for these applications. Our goal in this project is to develop a corneal OCT with one micrometer axial resolution, which could be used to quantify thickness profiles of the tear film and thin corneal layers in both normal and pathological corneas. We developed a spectral domain OCT using a broad bandwidth light (375 nm) from a supercontinuum source centered at 812.5 nm and a modified spectrometer design based on a Czerny Turner configuration to achieve ultrahigh (1.1 micrometer) axial resolution. In vivo images of human cornea representing our capability and potential ophthalmic applications are shown below.
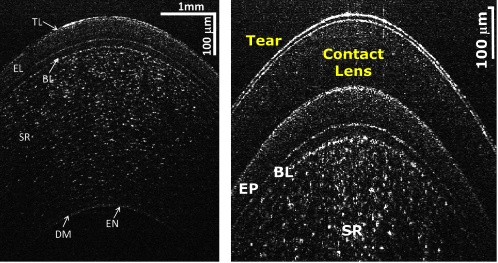
OCT image of the normal cornea visualizing different corneal layers, TL: Tear Layer, EP: Epithelium, BL: Bowman's Layer, SR: Stroma, DM: Descemet's Membrane, EN: Endothelium (left) and cornea with a soft contact lens on (right)
Histopathological analysis of the corneal diseases has provided valuable information on the mechanism of the diseases and for studying the cellular structural and functional changes with disease progression or therapeutic interventions. However, its invasiveness, potential artifacts induced during tissue preparation and the inability of sequential imaging of the evolving disease processes make it less desirable. In-vivo cellular imaging capability in cornea hence is desired as this can overcome the limitations mentioned above. The advent of in-vivo confocal microscope (IVCM) has enabled imaging of the cellular structure in the human and animal eyes in-vivo. Since its introduction IVCM has been successful in studying microstructural changes in the diseased corneas which includes changes in the density and shape of corneal cells with various diseases. However, since IVCM uses high NA objective lenses to achieve high axial and lateral resolution, its field size and working distance both are limited. It requires that the cornea be touched for measurement and it is almost impossible to monitor the same area of cornea at different time points. Standard OCT, although having large field and working distance, generally lacks the lateral resolution to image cellular structure in the tissue, as it uses small NA objective lenses to achieve higher imaging depth. Optical coherence microscope (OCM), a variation of OCT where a larger NA objective lens is used to improve the lateral resolution, has been shown to have the capability to image cells in the cornea ex-vivo. The high NA requirement however is not as pronounced in OCM as it is in IVCM, therefore it could be useful in overcoming the limitations of IVCM.
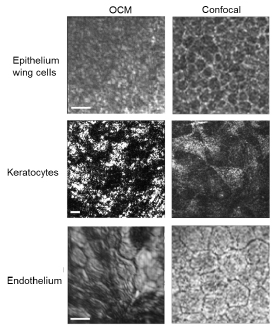
Comparison of different living mouse corneal cells imaged by OCM (left column) and in vivo corneal confocal microscope (right column).