
Advanced Physiological Optics Laboratory
Yoon Lab
Laser refractive surgery techniques such as photorefractive keratectomy (PRK) and laser in situ keratomileusis (LASIK) are surgeries designed to reshape the corneal surface in order to change the refractive state of the eye so that there is little to no further need for glasses or contact lenses. Corneal sculpting surgeries have been around for almost a century, but with the advent of the eximer laser, these types of corneal surgeries have become a popular option for people looking to correct myopia, hyperopia and astigmatism. Although these types of corneal surgeries are effective and safe, there is still much to be learned about how the cornea reacts and heals after these types of surgeries, and how best to perfect the programs that drive the lasers to give optimal vision for patients.
Laser refractive surgery is a technique in which a small laser beam (usually 2mm-6mm) is scanned across the surface of the cornea in order to ablate the surface tissue and change the shape and overall refraction of the cornea. The laser is scanned using a mirror which rotates around a central axis which creates an oblique incidence of the laser spot on the peripheral part of the ablation zone.
This oblique incidence results in a variable ablation rate depending on the ablation zone size and the curvature of the corneal surface. Due to this effect, actually induced defocus and spherical aberration are different from theoretically predicted values. This effect needs to be incorporated into a laser ablation algorithm to achieve better surgical outcomes.
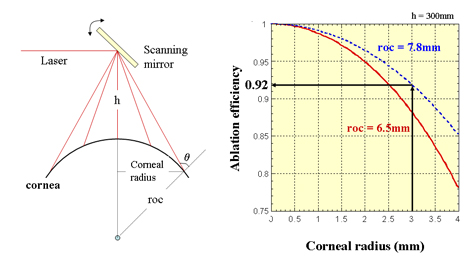
Figure 1: Schematic showing the oblique incidence of the laser beam on a curved surface (left), and the loss of laser ablation efficiency with varying radii of curvatures (right).
Understanding the results of laser refractive surgery has been a goal of the Yoon lab. We have worked to better understand the source of spherical type aberrations following refractive surgery (Yoon et al, J Cataract Refract Surg 2005; 31:127-135).
The graph below shows clinical patient data following refractive surgery (green dots) with respect to theoretically calculated data (red line) taking into account a variable ablation depth in the cornea, and biological healing responses in the cornea. The black dotted line is the predicted aberration changes calculated from well known algorithms that originally defined the laser algorithms, and the blue line is the predicted aberration changes taking into account just a variable ablation rate. It can be seen from this graph that actual clinical data can best be represented when taking into account both a variable ablation rate and biomechanical healing effects of the cornea. This leads to the need for a better understanding of how the cornea reacts to the laser ablations.
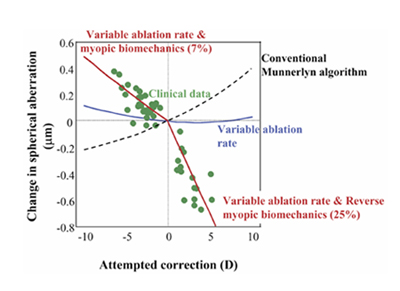
Figure 2: Clinical data showing that the change in aberrations with each attempted correction corresponds to the variable ablation rate of the laser and the biomechanics of the cornea.
Corneal crosslinking is an up and coming treatment which uses riboflavin solution and ultraviolet light to strengthen the corneal collagen fiber structure. Currently, this procedure is being used as an experimental treatment for keratoconus, and the crosslinking procedure has already seen some success in treatment of this disease. However, another effect of this treatment has been shown to be a thickening of the collagen fibers in the cornea. Our current avenue of investigation is into whether the corneal crosslinking procedure can be used to controllably, predictably, and selectively thicken the cornea as a refractive procedure.
We are now currently working to understand how the healing cornea changes the optical properties following surgeries such as LASIK and PRK. In collaboration with Drs Huxlin and MacRae, the Yoon lab has helped to establish a model to actively record wavefront measurements, along with optical coherence tomography (OCT), intraocular pressure, and corneal elasticity to better understand the optical and biological correlates in laser refractive surgery (Nagy et al. Photorefractive keratectomy in the cat eye: Biological and optical outcomes. 2007 JCRS 33 (6): 1051-1064). Through these studies it has been shown that following refractive surgery, a biomechanical factor - corneal stiffness, decreases, which may be a cause of post operative regression following surgery.
In addition we are currently working with our collaborators to better understand the cellular responses in the cornea that may be acting to keep the cornea soft following refractive surgery, in addition to further investigations into the exact biomechanical responses of the cornea to refractive surgery.